Supporting pregnant women who use alcohol and other drugs
Research staff: Courtney Breen, Emilie Awbery, Lucinda Burns
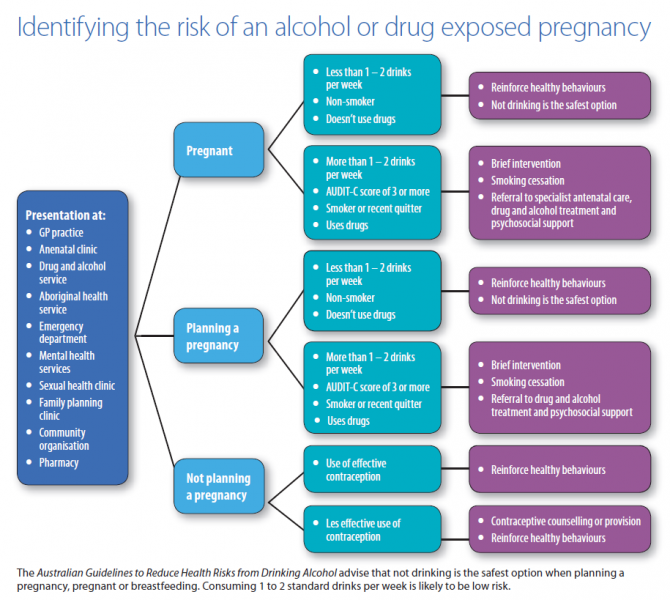
Interventions to reduce the risks of an alcohol or other drug exposed pregnancy can take place across the continuum from preconception, pregnancy and after birth. A framework to prevent exposed pregnancies and to minimise harm during pregnancy was developed to address risks across this continuum. The primary focus of the project was to identify strategies to identify and assist pregnant women who use or are dependent on alcohol or other drugs. In addition to assisting already pregnant women it is important to highlight that unintended pregnancy is associated with increased risk of exposure to alcohol or other drugs due to later pregnancy recognition, later access to antenatal care and higher likelihood of risky consumption patterns [1, 2]. Many unintended pregnancies occur due to inconsistent contraceptive use and therefore all women of reproductive age who use alcohol and other drugs should be provided with information and advice about effective contraception.
Substance use during pregnancy can be associated with significant harm to mother and baby. Health care professionals can make a substantial difference to the health of women and their babies by identifying and supporting women who use substances during pregnancy. It is important to remember that pregnant women who use substances are women who are dealing with all the complexities of substance use who become pregnant. Pregnancy may be a window of opportunity to motivate change and improve outcomes with the appropriate support and treatment. There is substantial stigma associated with substance use in pregnancy and this is a barrier for women accessing support [3].
Evidence suggests access to early antenatal care and access to specialist alcohol and drug treatment improves outcomes and therefore it is important to identify women that may need additional support as soon as possible [4]. Alcohol and drugs are used by women across the population, from a wide range of backgrounds and ages. A safe and non-judgemental approach is required to encourage disclosure and enable assistance with psychosocial and pharmacological treatment as required. Although evidence for universal screening is limited, guidelines recommend asking pregnant woman about their substance use within a discussion of their health [5]. Disclosure may occur as rapport is built and patterns of use may change over time, so it is important to continue to have this discussion throughout the pregnancy.
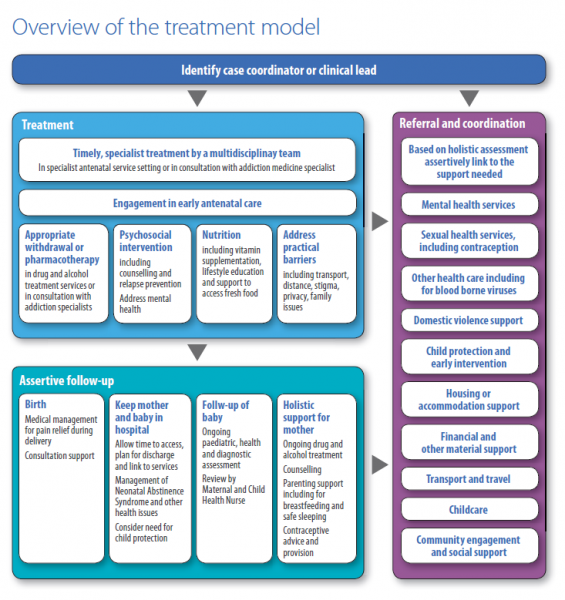
Moving beyond a focus on alcohol or drug use alone towards comprehensively addressing a range of factors improves outcomes [6] [7]. These include addressing early access to antenatal care, poor nutrition, mental health, domestic violence and unstable housing. Central to successful treatment responses are recognition of women’s experiences, including potential trauma, and provision of a compassionate model of care [8].
Best practice support of pregnant women who use substances:
|
Women may require psychosocial and/or pharmacological treatment depending on their individual needs. The type of treatment required varies by drug type. Clinical information by drug type is available from recently updated NSW Clinical Guidelines for the Management of Substance Use during Pregnancy, Birth and the Postnatal Period [9].
Pharmacological treatmentThere is a lack of high quality research into pharmacological interventions with pregnant women who use alcohol and other drugs [10, 11]. Due to this lack of rigorous research, the safety and efficacy of many treatments that are available to the general population are not known for pregnant women. Alcohol Benzodiazepines Tobacco Opioids Cannabis, Cocaine and Amphetamine Type Stimulants |
Psychosocial interventionsThere is a lack of high-quality research into psychosocial interventions with pregnant women who use alcohol and other drugs. Treatment should be trauma informed. Pregnant women with substance use disorders are a vulnerable population and many women may have a history of trauma. Cognitive Behavioural Therapy may assist with identifying and challenging dysfunctional thoughts and developing better coping strategies around substance use. There is some evidence for Motivational Interviewing reducing alcohol use in pregnant women. Developing relapse prevention skills may be particularly important for use in the postpartum period. There is some evidence for the use of contingency management in contributing to retention in treatment and reduction of drug use. |
Best practice approach
It is time and resource-intensive to support pregnant women with problematic alcohol or drug use, however health professionals can make a substantial difference to the outcomes of women and their babies. The project resource developed provides components of best practice information on how individual health professionals can support pregnant women, including addressing stigma and practical barriers. The resource describes important skills individuals should have or acquire, steps to take and directs health professionals to existing resources.
Skills which can support women’s engagement in care include:
- Understanding that alcohol or drug dependence is a health care issue and refraining from moral judgements.
- Being aware that alcohol and other drug use occurs in context of other health, family, cultural and psychosocial factors.
- Acknowledging that disclosing alcohol and other drug use during pregnancy can be difficult.
- Reflecting on one’s personal values.
- Building a trusting relationship over time.
- Acknowledging women’s experiences and feelings.
- Creating a safe, private and confidential environment.
- Providing a culturally safe environment.
- Understanding and addressing barriers to women accepting care.
- Being committed to providing optimum care.
Practical barriers to providing care need to be addressed and some strategies to overcome these include;
- Booking longer appointments or flexibility with appointment times.
- Anticipate missed appointments and follow up appropriately.
- Be opportunistic and arrange appointments with multiple disciplines for the same visit.
- Refer for a range of services to address practical issues such as transport, or be prepared to see women in range of community settings.
In addition the guide provides suggestions for service providers such as documenting information on local resources, referral pathways and to consider auditing the use of resources and clinical guidelines and putting quality improvement processes in place. Clarification of pathways between services and disciplines may be useful. An Australian study evaluated the implementation of a clinical pathway which aimed to improve outcomes for infants in families affected by alcohol or other drug use [16]. The pathway was multidisciplinary, with shared responsibilities and clearly articulated roles and responsibilities. Interventions focused on harm minimisation for substance use, parent-infant relationship, community support, mental health, wellbeing and stress management. The pathway appeared to facilitate a better therapeutic alliance between staff and families, improved engagement of women who were more likely to have an assessment, discuss substance use and have a safety plan regarding domestic violence. The intervention group remained engaged with the service longer than the control group [16].
Strategies to address organisational issues include [16-20]:
|
To ensure women get the appropriate support ongoing training of health professionals is required. There is lack of information and evaluation of the impact of education on practice. There is limited evaluation research of programs that treat pregnant women that use substances in Australia. Despite the availability of guidelines on screening and intervention for substance use in pregnancy, there is limited information on current practice or the extent to which guidelines are disseminated and implemented. Often funding is provided in stages and resource development occurs but the evaluation to determine the extent to which the guidelines and resources are used and their impact is not undertaken. This is an area that requires further attention to ensure that resources are being used effectively and women who use substances are supported throughout their pregnancy and beyond.
The project resources include:
- a fully referenced report,
- a practical guide for health professionals that contains information and links for resources including specialist antenatal clinics, guidelines, screening , assessment and intervention tools, domestic violence and contraception advice, Indigenous and youth specific resources.
- and a two page reference sheet
The project resources are available at https://ndarc.med.unsw.edu.au/resources.
Acknowledgments
Consultation network: The members of the consultation network, a range of professionals with interest and expertise in substance use in pregnancy, for their valuable input. They provided information on services available in their state, clinical practice in the identification and treatment of pregnant women who use substances, and workforce development needs. They gave input into the development of the resource, including its content, formatting and dissemination strategies.
Funding: The National Drug and Alcohol Research Centre, UNSW Australia, received funding for the Substance Misuse in Pregnancy Resource Development Project from the Australian Government
References
- Naimi, T., et al., Binge drinking in the preconception period and the risk of unintended pregnancy: Implications for women and their children. Pediatrics, 2003. 111(5 part 2): p. 1136-1141.
- Dott, M., et al., Association between pregnancy intention and reproductive-health related behaviors before and after pregnancy recognition, National Birth Defects Prevention Study, 1997–2002. Maternal and Child Health Journal, 2010. 14(3): p. 373-381.
- Gopman, S., Prenatal and Postpartum Care of Women with Substance Use Disorders. Obstetrics and Gynecology Clinics of North America, 2014. 41(2): p. 213-228.
- Wright, T.E., et al., Implementation and evaluation of a harm-reduction model for clinical care of substance using pregnant women. Harm Reduction Journal, 2012. 9(5): p. 1-10.
- World Health Organisation, Guidelines for the Identification and Management of Substance Use and Substance Use Disorders in Pregnancy 2014, World Health Organisation: Geneva.
- Ordean, A. and M. Kahan, Comprehensive treatment program for pregnant substance users in a family medicine clinic. Canadian Family Physician, 2011. 57(11): p. e430-e435.
- Milligan, K., et al., Birth outcomes for infants born to women participating in integrated substance abuse treatment programs: A meta-analytic review. Addiction Research & Theory, 2011. 19(6): p. 542-555.
- Poole, N., Bringing a Women's Health Perspective to FASD Prevention, in Fetal Alcohol Spectrum Disorder. 2010, Wiley-VCH Verlag GmbH & Co. p. 161-173.
- NSW Department of Health, NSW Clinical Guidelines for the Management of Substance Use during Pregnancy, Birth and the Postnatal Period 2014, NSW Department of Health: North Sydney.
- Smith, E., S. Lui, and M. Terplan Pharmacologic Interventions for Pregnant Women Enrolled in Alcohol Treatment. Cochrane Database of Systematic Reviews, 2009. DOI: 10.1002/14651858.CD007361.pub2.
- Bogenschutz, M.P. and C. Geppert, Pharmacologic Treatments for Women with Addictions. Obstetrics and Gynecology Clinics of North America, 2003. 30(3): p. 523-544.
- Jones, H.E., Treating opioid use disorders during pregnancy: historical, current, and future directions. Substance Abuse, 2013. 34(2): p. 89-91.
- Kaltenbach, K., V. Berghella, and L. Finnegan, Opioid dependence during pregnancy: effects and management. Obstetrics and Gynecology Clinics of North America 1998. 25: p. 139-151.
- Fajemirokun-Odudeyi O, et al., Pregnancy outcome in women who use opiates. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2006. 126(2): p. 170-5.
- Fisher, G., et al., Buprenorphine maintenance in pregnant opiate addicts. European Addiction Research 1998. 1: p. 32-6.
- Penny, R. and J. Pratt, The trial and evaluation of a clinical pathway for parents with substance use issues. Neonatal, Paediatric & Child Health Nursing, 2011. 14(3): p. 14.
- Jones, H.E. and K. Kaltenbach, Treating Women with Substance Use Disorders During Pregnancy: A Comprehensive Approach to Caring for Mother and Child. 2013: Oxford University Press.
- Pennay, A., D. Lubman, and M. Frei, Alcohol: prevention, policy and primary care responses. Australian Family Physician, 2014. 43(6): p. 356.
- Payne, J., et al., Changes in health professionals' knowledge, attitudes and practice following provision of educational resources about prevention of prenatal alcohol exposure and Fetal Alcohol Spectrum Disorder. Paediatric and Perinatal Epidemiology, 2011. 25(4): p. 316-327.
- NSW Department of Health, NSW Health Review of Substance Use in Pregnancy Services. 2009, NSW Health Mental Health and Drug and Alcohol Office North Sydney.










